Pulmonary abscess
General Information
Relevant disease coding (ICD10)
- A06.5+ Αμοιβαδικό πνευμονικό απόστημα
- J85 Απόστημα πνεύμονα και μεσοθωρακίου
- J85.0 Γάγγραινα και νέκρωση πνεύμονα
- J85.1 Απόστημα πνεύμονα με πνευμονία
- J85.2 Απόστημα πνεύμονα χωρίς πνευμονία
- J85.3 Απόστημα του μεσοθωρακίου
Types - Forms
Το πνευμονικό απόστημα μπορεί να κατηγοριοποιηθεί ως πρωτοπαθές και δευτεροπαθές:
- Πρωτοπαθές πνευμονικό απόστημα
- Παρουσιάζεται συνήθως σε υγιείς ασθενείς μετά από εισρόφηση και αποτελεί το 80% των περιπτώσεων
- Δευτεροπαθές πνευμονικό απόστημα
- Παρουσιάζεται συνήθως σε πάσχοντες ασθενείς από νοσήματα όπως:
- κακοήθεις νεοπλασίες
- ανοσοκαταστολή (π.χ. HIV)
- μετεγχειρητικές επιπλοκές
- Παρουσιάζεται συνήθως σε πάσχοντες ασθενείς από νοσήματα όπως:
Epidemiology
Impact - Prevalence
Δεν αναφέρονται σύγχρονα στοιχεία αναφορικά με την επίπτωση και τον επιπολασμό της νόσου. Αναφέρονται όμως τα πιο συχνά χαρακτηριστικά που παρατηρούνται σε ασθενείς με πνευμονικό απόστημα:
- προχωρημένη ηλικία
- ουλίτιδα
- κατάχρηση αλκοόλ
- παράγοντες κινδύνου για την αναρρόφηση
Παράγοντες Κινδύνου
- μειωμένη συνείδηση, όπως παρατηρείται σε:
- κατάχρηση αλκοολούχων ή ναρκωτικών
- αναισθησία και καταστολή
- νευρολογική δυσλειτουργία
- περιοδοντική νόσος
- διαταραχές κινητικότητας οισοφάγου
- γαστροοισοφαγική παλινδρόμηση
- δυσφαγία
- έμετος
- γαστρική υπερδιάταση
- καθετήρες σίτισης μεγάλου αυλού
- ανακλινόμενη θέση
- έμφραγμα μυοκαρδίου
- απόφραξη τραχειοβρογχικού δέντρου από νεοπλάσματα ή ξένα σώματα
- βρογχιεκτασίες
Related situations
- Νεκρωτική πνευμονία
- παρόμοια διαδικασία σχηματισμού με το απόστημα, μόνο που στην περίπτωση αυτή αρχικά σχηματίζονται πολλές μικρές κοιλότητες (<2cm σε διάμετρο) σε γειτονικές περιοχές μέσα στο πνευμονικό παρέγχυμα και προϊούσας της νόσου ενοποιούνται μεταξύ τους, σχηματίζοντας μία ενιαία κοιλότητα
- έχει παρατηρηθεί σε περιπτώσεις επιλοίμωξης μετά από γρίπη με ανθεκτικό στην μεθικιλλίνη χρυσίζοντα σταφυλόκοκκο
- Εμπύημα (περίπου το 1/3 των ασθενών με πνευμονικό απόστημα καταλήγει σε εμπύημα)
- Βρογχοπλευρική επικοινωνία
Reason - Pathogenesis
Reason
Οι κυριότεροι αιτιολογικοί παράγοντες δημιουργίας πνευμονικού αποστήματος είναι οι εξής:
- πολυμικροβιακές λοιμώξεις που σχετίζονται με εισρόφηση:
- συνήθως από αναερόβια μικρόβια
- αναφέρονται στο 85-93% των περιπτώσεων
- η είσοδος των μικροβίων προκαλείται συνήθως από διάσπαση του βλεννογόνου σε έδαφος ουλίτιδας
- συνήθως απομονώνονται οι εξής μικροοργανισμοί:
- Peptostreptococcus
- Prevotella
- Bacteroides
- Fusobacterium
- συνήθως από αναερόβια μικρόβια
- λοιμώξεις από αερόβια μικρόβια (συνήθως μονομικροβιακές):
- Streptococcus milleri (μπορεί να συμμετέχει και σε πολυμικροβιακή λοίμωξη)
- group A Streptococcus
- Staphylococcus aureus, συμπεριλαμβανομένου του μεθικιλλίνη ανθεκτικού στελέχους
- S. aureus (MRSA)
- Klebsiella pneumoniae
- Escherichia coli
- Pseudomonas aeruginosa
- Mycobacteria, συμπεριλαμβανομένου του Mycobacterium tuberculosis
- Nocardia, κυρίως σε ανοσοκατασταλμένους ασθενείς
- Rhodococcus
- λιγότερο συνήθη αίτια:
- παράσιτα
- Entamoeba histolytica
- Paragonimus westermani
- μύκητες
- Aspergillus
- Blastomyces
- Histoplasma
- Cryptococcus
- Zygomycosis
- παράσιτα
Pathogenesis
The most common way is a complication of pneumonia by aspiration:
- inoculation of microbes in the lung parenchyma by aspiration of large amounts of oral cavity fluids
- tissue necrosis occurs after 7-14 days and leads to the formation of the abscess
- in case the abscess communicates with the bronchial tree, purulent and smelly sputum is produced
Other ways of creating the lung abscess are:
- pulmonary embolism from septic emboli of the right heart chambers in the setting of infective endocarditis
- usually multiple abscesses are formed
- abscesses are formed in different (discontinuous) parts of the lung parenchyma
- haematogenous dissemination from purulent thrombophlebitis (e.g. Lemierre's syndrome)
Patient's personal history and clinical examination
Clinical picture
The clinical picture of pulmonary abscess due to anaerobic microbes includes the onset of subclinical symptoms, which may last for weeks, such as:
- cough, fever, purulent expectoration
- smelly sputum (indicating infection by anaerobic microbes) in 50% of cases
- in clinically confirmed pulmonary abscess from anaerobic microbes have been observed
- average temperature 38.9oC
- average white blood cell count in peripheral blood 15000/mm3
- average duration of symptoms to diagnosis about 14 days
- weight loss in 43% of cases
The clinical picture may be lightning-like in cases of Staphylococcus aureus or Klebsiella pneumoniae infection with symptoms such as:
- high fever
- leukocytosis
- early extension of the abscess to other lobes or to the pleural cavity
Individual background
Main symptom
- cough, fever, purulent expectoration
- additional symptoms:
- chest pain
- haemoptysis
- weight loss
History of present disease
Symptoms may be subacute or sluggish for weeks, and there may be a history of loss of consciousness or mental disorder.
Clinical examination
During the clinical examination, the following are found:
- fever
- poor oral hygiene and gingivitis
- cavernous or sandy breathing whispering
- absence of pharyngeal reflex
- keypad finger
Diagnosis
Diagnostic approach
- the chest X-ray shows a cavity with a hydraulic plane:
- usually with a thick wall
- there may be pulmonary infiltrates surrounding the cavity
- clinical findings supporting the diagnosis of aspiration lung abscess
- subclinical symptoms
- smelly sputum
- risk factors for causing aspiration
- clinical picture with a lightning strike usually associated with a monomicrobial infection by Staphylococcus aureus or Klebsiella pneumoniae
Microbiological diagnosis requires isolation of the pathogenic microorganism from sputum or other material of the bronchial tree and has:
- little benefit-usefulness in isolating anaerobic micro-organisms that are usually contaminated by the normal flora of the oral cavity and respiratory tract
- high utility-usability in identifying pathogenic micro-organisms causing monomicrobial infections
Differential diagnosis
The differential diagnosis includes the following conditions:
- Inspiration
- septic pulmonary embolism from infectious right ventricular endocarditis
- neoplasms, including:
- lung cancer
- non-Hodgkin's lymphoma
- metastatic carcinoma
- pulmonary embolism
- necrotic pneumonia
- tuberculosis
- knockout
- actinomycosis
- Rhodococcus
- Mycosis
- invasive aspergillosis
- blastomycosis
- histoplasmosis
- coccidiomyelitis
- cryptococcosis
- zygomycosis
- parasitism
- amoeba
- paragonimiasis
- echinococcosis
- necrotic pneumonia
- vasculitis
- granulomatous vasculitis
- lung disease in rheumatoid arthritis territory
- emphysematous cyst
- stinky stunts
Diagnostic tests
Imaging tests
The imaging tests that are usually performed to diagnose pulmonary abscess are:
- chest X-ray
- depicts a cavity with a hydraulic level:
- usually with a thick wall
- there may be pulmonary infiltrates surrounding the cavity
- depicts a cavity with a hydraulic level:
- chest CT scan
- can be more revealing than a simple X-ray
- the emergence of very small cavities
- in the identification of neoplastic lesions
- the distinction between abscess and fever
- can be more revealing than a simple X-ray
The American Thoracic Society (ATS) and the Infectious Diseases Society of America (IDSA) recommend that CT scans be performed in patients with pneumonia who do not respond to antimicrobial therapy, as CT scans:
- can distinguish pleural effusion from pulmonary thickening
- identify intraparenchymal abscesses, lymphadenopathy and solid lesions
In a published large series of patients diagnosed with pulmonary abscess the imaging findings were:
- unilateral lesions in 96.8% of cases
- simultaneous presence of pleural effusion in 9.5% of cases
- anatomical location of the abscess
- posterior part of the upper lobe or apical part of the lower lobe in 85.3% of cases
- basal parts of the lower lobe in 11.5%
- in the medial lobe or glottis at 3.2%
- diameter of the abscess
- <4cm at a rate of 15.9%
- 4-8cm at a rate of 66%
- >8cm at a rate of 18.3%
- 94% sensitivity
- 100% specialty
- 100% positive predictive value
- 94% negative predictive value


Chest X-ray with lung abscess
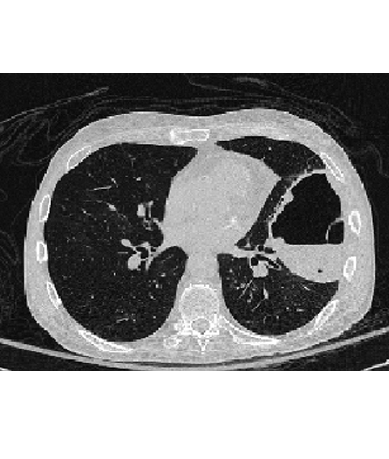
CT scan with lung abscess

Transthoracic ultrasound with lung abscess
Microbiological tests
Gram staining and sputum culture of patients with pulmonary abscess due to aspiration are characterized by:
- on Gram staining abundant neutrophils and complex microbial flora can be observed
- often in sputum there is an overgrowth of respiratory tract flora which makes it difficult to isolate pathogens
- for the collection of non-allocated biological material for cultivation (which is not often required) can be carried out:
- intertracheal suctions
- thoracocentesis
- transbronchoscopic bronchial lavage
- blood cultures (which are rarely positive for anaerobic infections)
- the usefulness of bronchoscopic bronchial lavage has not been documented
Gram stain and sputum culture appear to be more effective in patients with monomicrobial infections or when the pulmonary abscess is a secondary complication:
- anaerobic infections
- tuberculosis
- fungal infection
- parasitism
Treatment
Summary of the therapeutic approach
- first-line treatment is the administration of antibiotics
- the antibiotics given are similar to those given for the treatment of aspiration pneumonia
- το προτιμώμενο αντιβιοτικό σχήμα περιλαμβάνει αρχικά ενδοφλέβια χορήγηση κλινδαμυκίνης 600mg κάθε 8 ώρες (600mg X 3 iv), που ακολουθείται από του στόματος χορήγηση κλινδαμυκίνης 50-300mg κάθε 6 ώρες (50-300mg X 4 pos)
- alternative antibiotic regimens include:
- penicillin and metronidazole
- penicillin and a beta-lactamase inhibitor
- carbapenems
- quinolones with anaerobic activity, such as moxifloxacin
- targeted antibiotics based on an antibiogram, if the pathogen can be isolated
- the optimal duration of administration of the antibiotic regimen has not been determined
- usually, most patients are treated > 6-8 weeks
- the duration of treatment may be based on clinical and imaging response
- in patients who fail medical treatment, surgical treatment or percutaneous or endoscopic drainage of the abscess may be required
- no comparative studies have been conducted on early surgical treatment or invasive drainage of the abscess in patients at risk of failure of antibiotic treatment
Medication therapy
- antibiotic choice
- empirical treatment of pulmonary abscess
- το προτιμώμενο αντιβιοτικό σχήμα περιλαμβάνει αρχικά ενδοφλέβια χορήγηση κλινδαμυκίνης 600mg κάθε 8 ώρες (600mg X 3 iv), που ακολουθείται από του στόματος χορήγηση κλινδαμυκίνης 50-300mg κάθε 6 ώρες (50-300mg X 4 pos)
- alternative antibiotic regimens include:
- penicillin and metronidazole
- penicillin and a beta-lactamase inhibitor
- carbapenems
- quinolones with anaerobic activity, such as moxifloxacin
- targeted antibiotics based on an antibiogram, if the pathogen can be isolated
- empirical treatment of pulmonary abscess
- the optimal duration of administration of the antibiotic regimen has not been determined
- usually, most patients are treated > 6-8 weeks
- the duration of treatment may be based on clinical and imaging response
- some experts recommend continuing treatment until the chest X-ray "clears" or the imaged lesion remains small and stable
- clindamycin administration is associated with reduced treatment failure and reduced duration of disease symptoms, compared with penicillin administration in patients with anaerobic lung infections (level 2 [midlevel]evidence)
- clindamycin administration is associated with reduced treatment failure compared with metronidazole administration in patients with anaerobic lung infections (level 2 [midlevel]evidence)
Surgical treatment
- Surgical treatment is applied to patients who fail medical therapy.
- failure of medical treatment may be due to:
- large abscess cavity (>8cm)
- pathogen resistant to empirical antibiotic treatment (e.g. Pseudomonas aeruginosa)
- neoplasm blocking the communication of the cavity with the bronchial tree
- massive haemoptysis
- the most common surgical options include:
- lobectomy
- pneumonectomy
- limited pulmonary resection
- failure of medical treatment may be due to:
- Abscess cavity drainage
- percutaneous or endoscopic drainage is performed in patients where drug therapy has failed, neoplasia or other diagnosis is suspected and where the risk of surgical treatment is high
- percutaneous invasive procedures carry the risk of renewing the infection in the pleural cavity
- percutaneous transthoracic drainage with placement of a small catheter within the abscess is an alternative treatment to exploratory thoracotomy and lobectomy in patients with a pulmonary abscess that does not respond to medical therapy
- total mortality 4.8%
- complication rate 9.7%
- Inspiration
- haemothorax
- catheter obstruction
- thoracic
- percutaneous transthoracic drainage under CT guidance appears in a small series of patients to have a therapeutic effect of 83% and the main complication of pneumothorax in 13%
- percutaneous transthoracic drainage with placement of a small catheter within the abscess is an alternative treatment to exploratory thoracotomy and lobectomy in patients with a pulmonary abscess that does not respond to medical therapy
- endoscopic drainage can treat pulmonary abscess in patients where drug therapy has failed and is performed by transbronchoscopic (through the nose) placement of a pigtail catheter into the abscess cavity and daily flushing of the cavity with antibiotic solution
- endoscopic drainage is not widely accepted because of the risk of transferring pus and necrotic material to healthy parts of the lung, potentially leading to acute respiratory distress syndrome (ARDS)
Patient monitoring
Patients are followed up with clinical examination and imaging tests for as long as necessary, as the optimal duration of the antibiotic regimen has not been determined:
- usually, most patients are treated > 6-8 weeks
- the duration of treatment may be based on clinical and imaging response
- some experts recommend continuing treatment until the chest X-ray "clears" or the imaged lesion remains small and stable
Complications and prognosis
Complications
Pulmonary abscess in case of inadequate treatment can cause:
- Inspiration
- bronchopleural fistula
- pneumocele
- haemoptysis
- respiratory distress syndrome
- metastatic brain abscess
- pneumothorax
- amyloidosis
Forecast
- morbidity and mortality has been significantly reduced with the use of antibiotics
- fever may persist for 4-8 days after starting medication
- the radiographic picture may initially show deterioration
- the majority of patients (85-90%) show improvement with the start of drug therapy
- modern studies report:
- 1% mortality in a large series of 205 patients from Japan (1994-2008)
- 20% mortality in a smaller series of 75 patients from Israel (1980-1996)
- 83% mortality when the causative agent was Pseudomonas aeruginosa
- 50% mortality when the causative agent was Staphylococcus aureus
- 44% mortality when the causative agent was Klebsiella pneumoniae
Prevention and population control
Prevention
The effort to prevent the occurrence of pulmonary abscess consists mainly in the prevention of aspiration episodes and subsequent aspiration pneumonia.
Guidelines
- United States guidelines
- Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia.
- Adult hospital and ventilator-associated pneumonia guidelines: eminence- rather than evidence-based.
- Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists Committee on Standards and Practice Parameters.
- United Kingdom guidelines
- Asian guidelines
