Pectus excavatum
Description
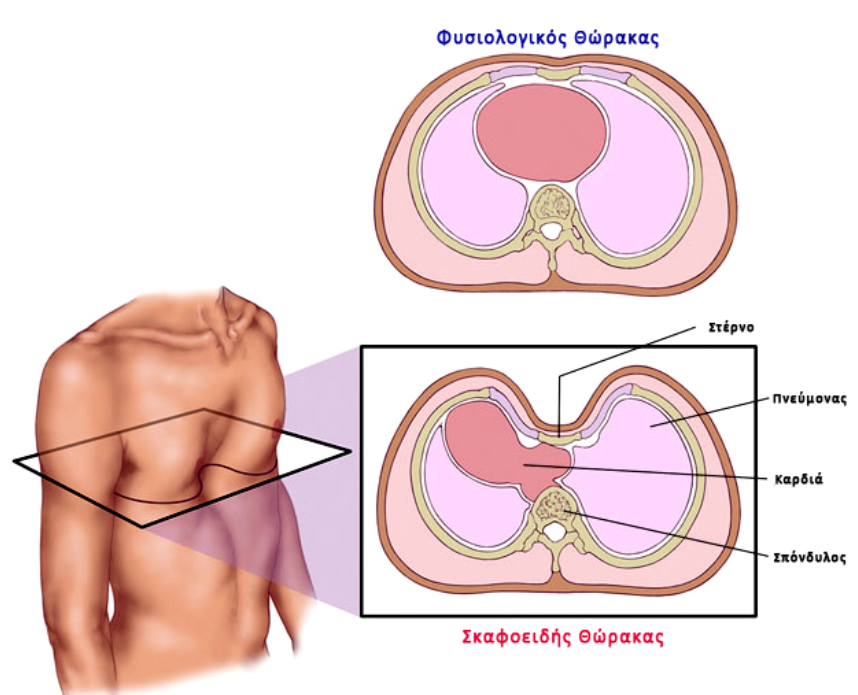
Pectus excavatum (pectus excavatum) or chanoid chest or shoemaker's chest is a chest wall deformity characterised by posterior (inward) depression of the sternum and adjacent lateral cartilage. Scaphoid sternum is the most common congenital chest wall deformity and occurs more frequently in males. In addition to the aesthetic disorder, this deformity may exert pressure on the heart and lungs. In the majority of cases it occurs from the first year after birth, the rest during early adolescence. In infancy and childhood usually the deformity does not usually result in any symptomatology. During prepubertal and adolescent years, typically the deformity worsens due to rapid physical growth and cardiorespiratory symptoms such as dyspnoea and exercise intolerance occur. The main reason for the development of scaphoid sternum is unknown, but approximately 40% of patients have a positive family history of chest wall deformities and it is usually associated with other musculoskeletal or connective tissue diseases, such as scoliosis, Marfan syndrome, Ehlers-Danlos syndrome and incomplete osteogenesis.

Epidemiology
Scaphoid sternum is more common in males (male/female 5:1). It occurs in 86% in the first year of life. The incidence is about 1 in 400 births.
Reason
The cause of congenital scaphoid sternum is unknown.
Acquired sternal scaphoid usually results from postoperative complications after thoracic surgery, such as after surgical repair of congenital diaphragmatic hernia (33% after repair of congenital, posterior diaphragmatic hernia.
Pathogenesis
Scaphoid sternum may occur due to abnormal congestion of the diaphragm in the sternum and weakening of the lateral cartilage. Abnormalities of the lateral cartilages that have been found to be associated with their weakening include abnormal collagen solidification and distribution, perichondritis, areas of aseptic necrosis, decreased zinc concentration and increased magnesium and calcium concentration. This abnormal weakening of the lateral cartilage in the pleural joints results in posterior migration of the sternum. The development of dysmorphism brings about disturbances in the function of the respiratory muscles and exerts a compressive action on the heart and lungs resulting in:
- impaired respiratory function
- deformation and dysfunction of the heart
- mitral valve prolapse and concomitant failure
- deformation of the right ventricle of the heart with impending reduced filling and reduced ejection fraction
- heart rhythm abnormalities
The underlying symptomatology is exercise intolerance and dyspnoea during exercise.
Clinical picture
Symptoms usually appear during the sudden physical growth in adolescence. The most common are:
- Exercise intolerance
- Shortness of breath during effort
- Reduced strength
- Palpitations
- Chest pain
At the same time there are concerns about the aesthetics of the body's appearance.
These symptoms worsen as children develop more sporting activities and in cases where the deformity is very severe they develop into:
- Shortness of breath at the slightest effort
- Wheezing exacerbated by exercise
- Fainting/dizziness
- Tachycardia
- Inability to follow the activities of his/her peers
- Common upper respiratory tract infections
- Psychosocial difficulties
Clinical examination
Chest
Carrying out a medical assessment:
- the degree of depression of the sternum and the lower rib cartilages
- the symmetry or asymmetry of the deformity in the two halves
- the twisting of the sternum
- the point of maximum immersion
Heart
Cardiological assessment including:
- disorders of the heart rhythm
- mitral valve prolapse
Musculoskeletal
Check for the presence of scoliosis.
Diagnosis
The diagnosis is mainly based on clinical examination and when clinically severe dysmorphia is diagnosed, then it is decided to perform further imaging tests, detailed cardiological and respiratory examination in order to accurately determine the degree of dysmorphia and its influence on cardiorespiratory function.
Diagnostic tests
- Chest CT
- assessment of the severity of the deformity by calculating the Haller index (transverse internal diameter of the thoracic cage / shortest sternoclavicular depth), where Haller index > 3.25 means severe deformity
- assessment of the deformity of the lateral cartilages
- assessment of the symmetry of the thoracic cage
- assessment of heart and lung compression
- assessment of the relationship of the immersed sternum on the compressed heart
- Spirometry
- assessment of restrictive and obstructive respiratory dysfunction
- Hypercardiogram
- assessment for cardiac compression and paralysis
- assessment for mitral valve prolapse and mitral regurgitation
- MRI of the chest - heart can replace CT and echocardiography (and at the same time avoid radiation exposure)
Treatment
Treatment of scaphoid sternum is indicated for symptomatic patients or for aesthetic reasons. In theory, two or more of the following criteria must be met:
- Haller index > 3.25 (associated with cardiorespiratory compression)
- Restrictive or obstructive type lung disease
- Cardiac compression and misalignment causing mitral valve regurgitation or arrhythmias
- Progressive deterioration of deformity
Non-surgical treatment
Σύμφωνα με τα πιο πρόσφατα βιβλιογραφικά δεδομένα του 2019, η καταλληλότερη ηλικία για την μη χειρουργική επιδιόρθωση είναι μεταξύ 8-12 χρονών όταν δεν έχει ακόμα ολοκληρωθεί η ανάπτυξη του θωρακικού κλωβού. Η θεραπεία αφορά την εφαρμογή μιας συσκευής κενού (vacuum bell device) που αναπτύχθηκε το 2005 από τον Eckart Klobe.

With this technique, suction is used to retract (outward) the immersed lower third of the sternum and the lateral cartilage so that the thoracic cage can acquire its normal shape. The application of the treatment is carried out daily by the child's parents after appropriate training by a qualified thoracic surgeon. Usually the initial application takes 10-15 minutes of an hour twice a day and the daily treatment time is gradually increased to 3-4 hours a day. According to the results of large international patient series, it usually takes 18-24 months for 80% improvement of the scaphoid sternum. Treatment efficacy is related to the age of onset of treatment (<11 years), depth of sternal depression (1 year) (Nonoperative management of pectus excavatum with vacuum bell therapy: A single center study, 2018, USA).
Surgical treatment
The most appropriate age for surgical repair is between 15-16 years old, just before the skeleton has finished developing. There are two modern surgical repair techniques:
- Intervention by Nuss
- It is essentially two procedures, one for the thoracoscopic placement of a metal bar that lifts the sternum and a second procedure after 2-3 years to remove the bar. It has very good results in symmetrical deformities.
- Ravitch intervention
- This is a single open surgery in which all the lateral cartilage causing the deformity is removed. It is indicated for all deformities, even asymmetrical or more complex ones, and for people who do not want two surgeries or the implantation of a metal bar.
You can arrange an appointment with the doctor
In the morning the Thoracic Surgeon, Dr Athanasios Kleontas MD is at the Interbalkan Medical Center of Thessaloniki, while in the evening he is at his private office (73, Ermou St).
+30 2310 - 400000
Office 11, 2nd floor. Dec 1742
ATHANASIOS D. KLEONTAS
PATIENT VISITATION HOURS
Doctor is available (by mobile) 24 hours a day, 7 days a week.
You meet him only by appointment at his private office:
Monday to Friday : 18.00 - 21.00




