Pneumothorax
Brief presentation of spontaneous pneumothorax and treatment (click)
Παρουσίαση κλινικού περιστατικού με αυτόματο πνευμοθώρακα
Definition
Auto pneumothorax (spirit = air + chest) is the non-traumatic collection of air within the pleural cavity.
Types
- Primary spontaneous pneumothorax (PSP), which is not associated with clinically evident lung disease.
- Secondary spontaneous pneumothorax (SSP), which is associated with clinically evident lung disease.
Epidemiology
Primary spontaneous pneumothorax usually occurs in tall and thin people, aged 15-34 years. It rarely occurs in people older than 40 years. Secondary spontaneous pneumothorax occurs mainly in patients with underlying lung disease, usually in people older than 55 years. The reported incidence is 6.3-24/100000 per year for men and 1.2-9.8/100000 per year for women.
The most likely risk factors for spontaneous pneumothorax are:
- smoking (dose-dependent relationship)
- pneumonia due to pneumonocystis jirovesi (especially in patients with HIV)
- occupations or sports related to changes in atmospheric pressure, such as aircraft pilots and divers
Causal factors
The main causes of air collection within the pleural cavity are as follows:
- Primary spontaneous pneumothorax from spontaneous rupture of pulmonary or subpulmonary emphysematous cysts into the pleural cavity
- Secondary spontaneous pneumothorax that can be caused by underlying lung disease such as:
- Obstructive lung disease
- chronic obstructive pulmonary disease (most common cause)
- acute, severe asthma
- κυστική ίνωση
- Infectious lung diseases
- pneumonia from pneumonocystis jirovesi
- necrotic pneumonia
- tuberculosis
- Interstitial lung diseases
- sarcoidosis
- idiopathic pulmonary fibrosis
- Histiocytosis X
- lymphangioleiomyomatosis
- Diseases of the connective tissue
- rheumatoid arthritis
- scleroderma
- Marfan syndrome
- Ehlers-Danlos syndrome
- ankylosing spondylitis
- idiopathic inflammatory myopathy (polymyositis/dermatomyositis)
- Cancer of the lung
- Endometriosis (emphysematous pneumothorax)
- Sarcoma involving the lung
- Obstructive lung disease
- Rupture of the oesophagus
- Birt-Hogg-Dube syndrome (a rare, autosomal, predominant disease affecting the skin and lungs that increases the risk of multiple benign tumours
- Changes in atmospheric pressure (pilots and divers)
- Individual rare cases
Pathogenesis
The interpretation of the pathogenesis of spontaneous pneumothorax is based on the following hypotheses:
- the degradation of pulmonary elastic fibres promotes the formation of subpulmonary emphysematous cysts
- the presence of emphysematous cysts promotes inflammation leading to the obstruction of small airways
- an increase in intra-alveolar pressure to levels higher than the intrapulmonary pressure results in air escaping from the alveoli into the pleural cavity
Very small (blebs) or larger (bullae) emphysematous cysts have been found in 94% of patients with recurrent or complicated spontaneous pneumothorax. Primary pneumothorax may be familial.
Symptoms
Symptoms usually present suddenly and may be mild or absent. The most common symptoms are:
- Shortness of breath
- Chest pain
- sudden
- Acid
- unilateral
- localized on the sides
- greater intensity at the start
- usually sets after 24h
It has also been observed that 87% of patients were not doing any activity at the onset of symptoms, 9% of patients were doing some sudden movement, while only 2% were doing some vigorous activity. In catamenial pneumothorax, the symptoms occur during menstruation, and there are usually concomitant symptoms of endometriosis. Symptoms of cardiorespiratory dysfunction are usually due to tension pneumothorax.
Clinical examination
- reduced development of the mediastinum
- transcendence in impact
- reduction or absence of respiratory depression
Diagnostic approach
- Imaging control
- Chest X-ray
- Chest CT
- Transthoracic ultrasound

Chest X-ray
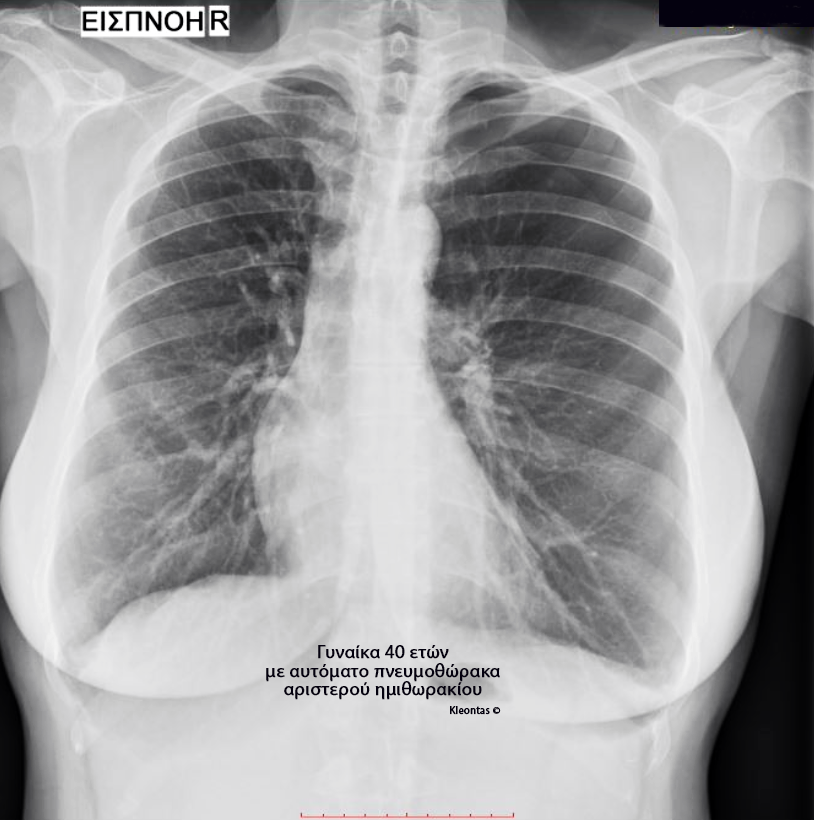
Chest X-ray

Computed tomography of the chest
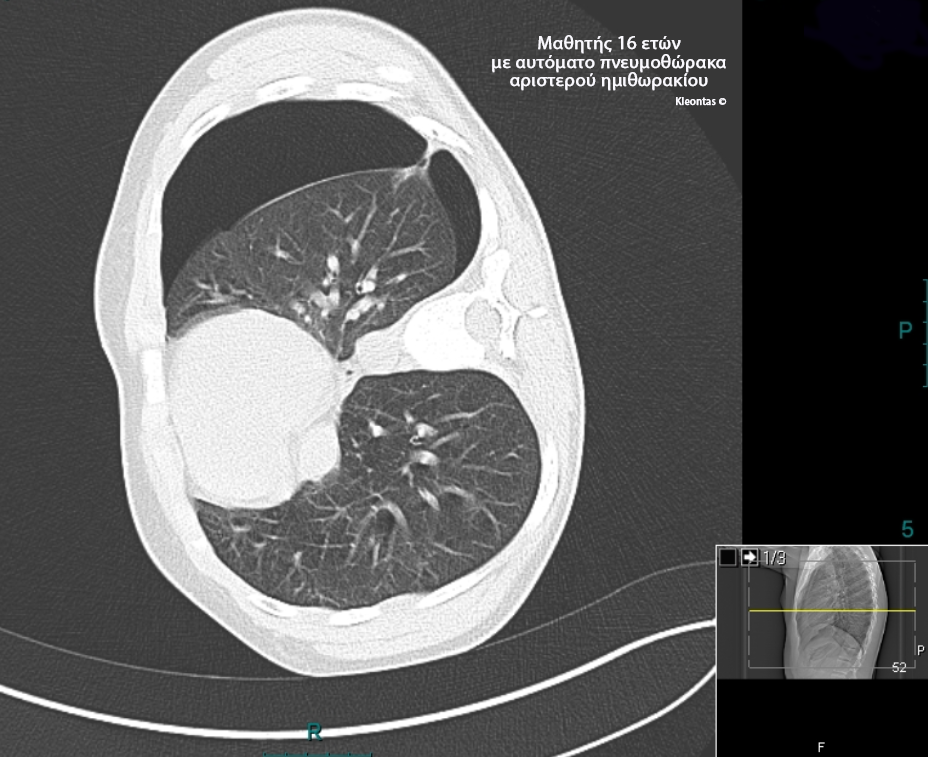
Computed tomography of the chest
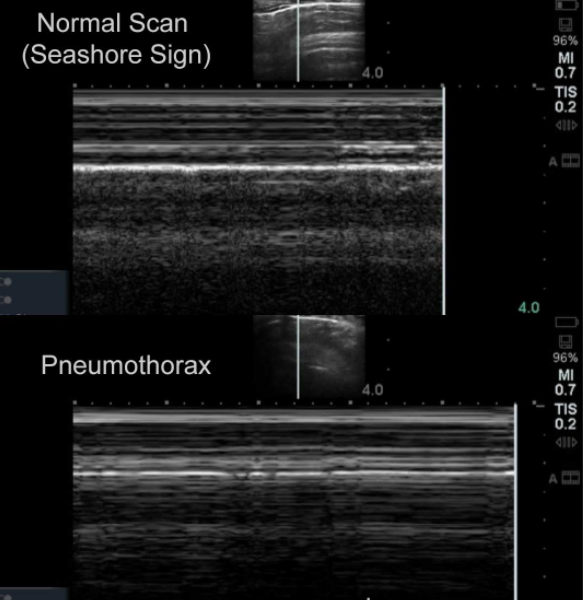
Transthoracic chest ultrasound
Address
General recommendations
- In case of tension pneumothorax, immediate drainage is recommended
- Monitoring is suggested for:
- patients with small spontaneous pneumothorax (distance between free lung boundary and chest wall < 2cm) and non-significant dyspnoea
- selected, asymptomatic patients with large spontaneous pneumothorax (distance between free lung boundary and chest wall > 2cm)
- High flow oxygen administration to all patients
- Hospital admission of all patients with secondary spontaneous pneumothorax
- Interventional treatment is recommended in all patients with primary or secondary spontaneous pneumothorax and dyspnoea related to the extent of the pneumothorax
- pneumothorax drainage by the insertion of a needle, catheter or chest tube
- needle drainage can be as effective as tube insertion and thus reduce hospital days
- pleurodesis with pleurodesis agent through the chest tube or thoracoscopically (VATS)
- chemical pleurodesis is suitable for patients who are unable or do not want surgical treatment
- pneumothorax drainage by the insertion of a needle, catheter or chest tube
- For patients with recurrent spontaneous pneumothorax it is recommended:
- pleurodesis with pleurodesis agent through the chest tube or thoracoscopically (VATS)
- thoracoscopic talc infusion reduces the recurrence rate compared to talc injection through the chest tube
- pleurodesis with minocycline infusion reduces the recurrence rate and subsequent thoracoscopic procedures
- surgical treatment
- for difficult or recurrent pneumothoraces, open access and pleurectomy has the lowest recurrence rate (1%)
- the thoracoscopic approach compared to the open approach has similar results
- pleurodesis with pleurodesis agent through the chest tube or thoracoscopically (VATS)
- The treatment of catamenial pneumothorax involves a combination of surgery and hormone therapy
Surgical treatment
Pneumothorax drainage with needle insertion into the affected hemithorax
- 14-16 G needle placement is just as effective as larger gauge needles (>20 G)
- Needle drainage in the emergency department can reduce hospitalisation time compared to chest tube insertion
- Needle drainage can be as effective as chest tube drainage and can reduce hospitalisation time
- Needle drainage and small chest drainage catheter placement appear to have the same failure rates in the treatment of spontaneous pneumothorax
- There are no comprehensive randomized trials comparing conservative and interventional treatment of spontaneous pneumothorax
Pneumothorax drainage with placement of a chest drainage tube in the affected hemithorax
- The use of a small diameter chest tube is usually required
- Recommended in patients with secondary spontaneous pneumothorax
- Recommended in patients with tension pneumothorax or bilateral pneumothorax
- When it is necessary to connect the drainage pipe to a suction (not always required), it is recommended to use high-volume and low-pressure suction suction systems
- Heimlich valve connection to the drainage tube has a reported 86% efficacy in the treatment of pneumothorax
- Early and aggressive treatment is recommended in patients with cystic fibrosis and the onset of pneumothorax
- Chest tube insertion is associated with higher success rates compared to needle drainage, but there is no difference in the recurrence rate in the first three months
Thoracoscopic and open treatment
- Thoracoscopic resection of the pleural wall (pleurectomy) with synchronous mechanical abrasion of the visceral pleura is better tolerated by patients compared to open thoracotomy and pleurectomy, but with a higher recurrence rate (5%)
- Subsequent mechanical pleurodesis (with pleural friction) after thoracoscopic wedge resection (usually of the top of the lung) does not reduce the recurrence rate of primary spontaneous pneumothorax
- Comparison of the thoracoscopic with the open approach
Pleurisy
- Chemical pleurodesis is effective in treating difficult and recurrent cases of pneumothorax
- The most commonly used pleurodesensitising agents are talc, doxycycline, tetracycline and minocycline
- Preferably blowing 5gr of talc to achieve chemical pleurodesis
- Thoracoscopic talc infusion reduces the rate of pneumothorax recurrence compared with simple drainage with chest tube insertion
- Chemical pleurodesis with talc may be associated with respiratory complications
- Chemical pleurodesis with minocycline reduces the recurrence rate and subsequent thoracoscopic interventions
- Chemical pleurodesis with minocycline after thoracoscopic intervention may increase analgesic use but reduce the relapse rate
- Chemical pleurodesis with minocycline has the same recurrence rates as partial pleurectomy of the semithoracic dome, but increased analgesic use
Complications of pneumothorax
- under tension pneumothorax
- bronchopleural fistula
- ex vacuo pneumothorax (non-regrowth of the lung)
Forecast
Secondary spontaneous pneumothorax is associated with higher morbidity and mortality than primary spontaneous pneumothorax
Guidelines
- British Thoracic Society (BTS) guidelines
- European Respiratory Society (ERS) task force statement
- American College of Chest Physicians (ACCP) consensus statement
You can arrange an appointment with the doctor
In the morning the Thoracic Surgeon, Dr Athanasios Kleontas MD is at the Interbalkan Medical Center of Thessaloniki, while in the evening he is at his private office (73, Ermou St).
+30 2310 - 400000
Office 11, 2nd floor. Dec 1742
ATHANASIOS D. KLEONTAS
PATIENT VISITATION HOURS
Doctor is available (by mobile) 24 hours a day, 7 days a week.
You meet him only by appointment at his private office:
Monday to Friday : 18.00 - 21.00
